Arthritis in horses is a degenerative joint disease of the equine family, which involves the joints and cartilages manifested by pain in legs and ultimately leads to lameness. Another name of the equine arthritis is Degenerative Joint Disease (DJD), joint disease or osteoarthritis, or bone sprain or laminitis. There are mainly two types of arthritis in horses like traumatic arthritis and septic arthritis.
Traumatic Arthritis
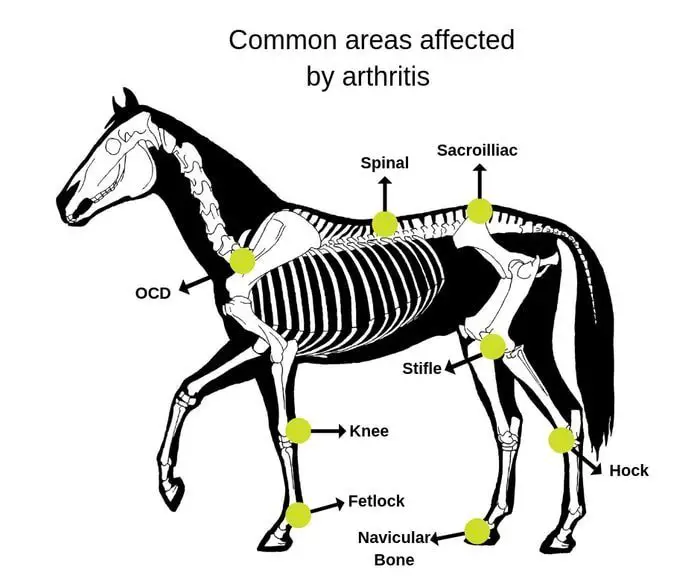
Traumatic Arthritis and degenerative arthritis are frequently closely linked. There are few occasions when a single traumatic incident will be the initiating factor in the development of arthritis. Examples of this include displaced intra-articular fractures, such as the olecranon, condylar, and some sesamoid fractures. Most frequently, low-grade repetitive trauma initiates a destructive cycle that results in DJD. Arthritis in horses is most commonly encountered in joints such as the carpus and fetlock but may be seen in any site. Traumatic arthritis also includes synovitis, capsulitis, and articular cartilage damage, and it is, therefore, complicated to separate chronic traumatic form degenerative arthritis.
Septic Arthritis in Horses
The entry of bacteria into a joint can occur as a result of hematogenous spread by penetrating injuries, by extension from adjacent soft tissue or osseous lesions, as a consequence of intra-articular injection or as a complication of surgery.

What are the Causes of Equine Arthritis
Septic arthritis in foals is usually referred to as joint ill. In such cases, a focus of infection can usually be found elsewhere in the foal, such as an infected umbilicus. Foals with joint ill are frequently immunocompromised, and multiple joints may be affected. The spread of infection is usually via the hematogenous route.
In adult horses penetrating injuries and injections are the most common cause of septic arthritis. Drugs such as PSGAG and cortisone are most frequently involved. Septic arthritis may occur in any joint.

How do I know if my horse has arthritis?
The appearance of clinical signs can often be delayed for several days after the initial infection and can extend up to 7 days after a cortisone injection, which has the effect of initially diminishing the clinical response. Horses with septic arthritis are usually severely lame, with pain on palpation or flexion of the affected joint. There is usually marked swelling of the joint, which also has a thickened joint capsule. Affected horses are usually depressed and have a decreased appetite. They may be pyrexia.

Sometimes low-grade septic arthritis and synovitis occur. Affected horses are moderately lame, but have severe synovitis and effusion, as well as pain on palpation of the joints, which are often very warm to touch.such horses may respond temporarily to treatment but frequently relapse. They are moderately depressed and often have only a slight temperature rise, to about 38.1-38.4° C.
Pathophysiology of Equine Arthritis
Once an infection enters the joint, the synovial membrane responds by becoming inflamed, resulting in the production of increased amounts of synovial fluid and the liberation of degradative enzymes. These enzymes result in glycosaminoglycan, proteoglycan and collagen loss from the cartilage, and subsequent erosion of the articular surface. The formation of fibrin clots in the joint further compromises synovial membrane function, as well as interfering with the nutrition of the articular cartilage. If full-thickness cartilage loss occurs and the subchondral bone is penetrated by bacteria, septic osteomyelitis will develop. Conversely, osteomyelitis or septic physitis can extend into a joint and initiate septic arthritis. In such cases, the radiographic abnormalities in the subchondral bone are much more severe early in the course of the disease than would be expected if septic arthritis had been the initiating factor.

Diagnosis of Arthritis in Horses
This is based on clinical signs and joint fluid analysis. The only other condition that will result in as much joint pain is a fracture. Therefore if a fracture is excluded, it is almost certain that joint sepsis is present. Strong consideration should be given to a diagnosis of joint sepsis if the synovial fluid has a protein content of greater than 30 g/L and a white cell count greater than 5000/micro L, of which 90% are neutrophils. However, values less than these do not preclude a diagnosis of septic arthritis. The infected joint fluid will also usually have a serosanguinous or seropurulent appearance. Joint fluid from horses with very low-grade, or chronic sepsis, can often appear relatively normal grossly. Samples should be submitted for bacteriology. The culture of organisms from infected joints can often be unrewarding; however, inoculation of enhancement broths can improve this.
Radiography may reveal evidence of gas within joints or fractures associated with the sepsis or its initiating factors. In longstanding cases, evidence of severe secondary DJD will be apparent radiographically.
How do you treat arthritis in horses?
- Early and aggressive treatment is required. If possible arthroscopic examination of the joint should be performed.
- This enables a thorough examination and removal of any fibrin clots and other debris. Most importantly, it allows extensive lavage of the joint.
- If arthroscopy cannot be performed, lavage via a 10-14 gauge catheter should be performed.
- An ingress and egress catheter should be placed on either side of the joint, and 10-15 L balanced polyionic solution flushed through. Saline should be avoided, as this can be irritant to articular cartilage and synovial membrane.
- During flushing, the egress cannula should be frequently closed to allow distension irrigation of the joint.
- The use of intra-articular medication is controversial. The main objection has been that the drugs used will create synovitis and thus harm articular cartilage.
- However, in view of the severity of the disease process induced by the sepsis, the additional synovitis is probably minimal.

- The advantage of intra-articular medication is that higher drug levels are present in the joint that can be achieved via systemic administration.
- The most frequently Intraarticular drugs are amikacin (1 g intra-articularly) and gentamycin(300-500 mg intra-articularly).
- Other medications that may be used include povidone-iodine and DMSO. Ten to 20 l dilute povidone-iodine (0.5%) may be flushed through the joint as an alternative lavage solution. Five to 10 L DMSO in a 20-40% solution may also be used.
- In refractory cases, a lavage tube may be inserted into the joint, with a 1 cm exit portal created on the opposite side of the joint, which is left open. Lavage solution can then be flushed through under gravity flow for 24-48 h.
- Open joint wounds should be protected by sterile bandages, which may need to be changed twice daily if the extensive discharge occurs.
- Systemic medication is also indicated. Ideally, antibiotics should be selected as a result of culture and sensitivity patterns.
- Prior to this information being available, or if culture is unsuccessful, penicillin and gentamicin, or potentiated sulphonamides are indicated.
- Procaine penicillin should be administered IM at a dose rate of 15 mg/kg b.i.d., while1-3 mg/kg of gentamicin IV two or three times daily is indicated.
- Benzylpenicillin is a suitable alternative to procaine penicillin. Up to 30 mg/kg of trimethoprim-sulpha combinations twice daily may be given, either PO or IV.
- NSAIDs are recommended.
- Phenylbutazone at a dose of 4.4 mg/kg, reducing to 2.2 mg/kg in the first 3-4 days, is most useful and should be continued for at least a week after clinical signs have resolved. Up to 3 wks, additional treatment is recommended in foals, where a focus of infection is often located distant from the site of joint sepsis and needs to be located and treated appropriately.
- In refractory cases, consideration should be given to arthrodesis joints. This has the effect of eliminating the joint space and synovial membrane and is often the only means of resolving some septic joint problems.
- It is essential to realize that septic joints are an emergency, and often require prolonged medication, and possibly repeated surgical intervention if a successful outcome is to be achieved. Owners should be advised of this before treatment is instituted.
Prognosis of Equine Arthritis
The earlier in the course of the disease treatment is initiated, the better the chances of a successful resolution. If sepsis has been present for 14 days or more, the chances of successful long term resolution are low. Even if the infection is controlled, cartilage damage may be severe enough to render the horse chronically lame.